The Gut-Brain Axis: The Intricate Connection Between Mental Health and Gut Health
In our integral approach to understanding health, it is vital to explore the intricate relationship between mental health and gut health – often referred to as the 'gut-brain axis'. In the past decade, substantial scientific research has started to unravel this complex interplay, conclusively demonstrating that disturbances in either system can profoundly influence the other.
The Interaction Between Mental Health and Gut Health
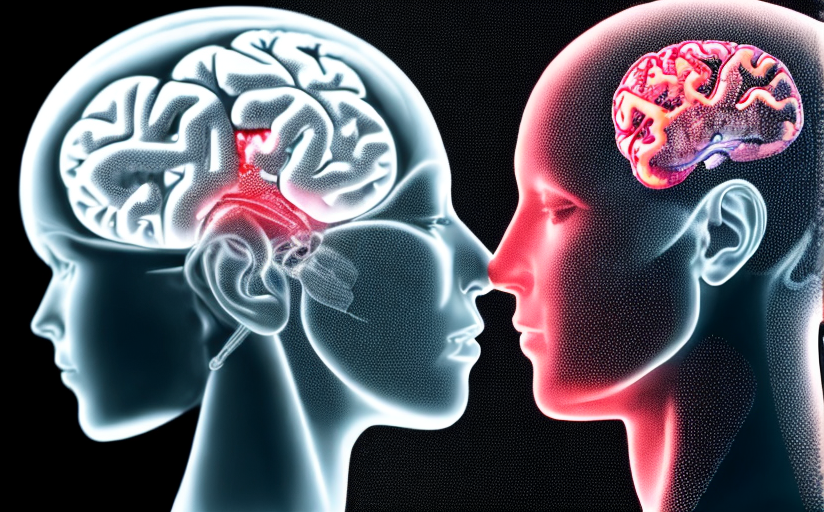
Gut health and mental health are not separate entities. They are closely interconnected through a bidirectional communication network termed the 'gut-brain axis'. This concept simply means that your gastrointestinal tract, or gut, communicates with your central nervous system, which comprises the brain and the spinal cord. This communication happens through various paths including neural, endocrine, and immune pathways.
Emerging evidence indicates that a healthier gut corresponds to better mental health, and an impaired gut can significantly contribute to mental disorders. According to several studies, conditions like anxiety, depression, autism, schizophrenia, and even Parkinson's disease can be closely linked to the state of our gut health.
The Role of Microbiota in the Gut-Brain Axis
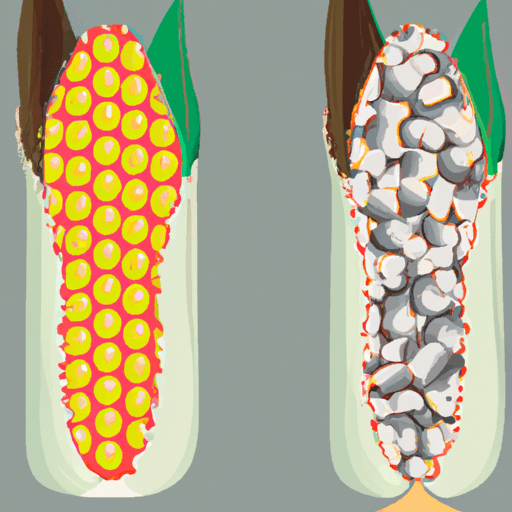
Playing an essential role in the gut-brain axis are our gut microbiota – the complex community of trillions of bacteria and other microbes that inhabit our gastrointestinal tract. The gut microbiota can influence the brain and behavior by producing various neurotransmitters and metabolites that can cross the blood-brain barrier. For instance, it is known that 90% of our body's serotonin - a neurotransmitter that helps regulate sleep, appetite, moods, and inhibit pain - is produced in the gut by certain species of gut bacteria.
Scientific research is now beginning to show that alterations in the composition and function of the gut microbiota - called dysbiosis - could significantly impact mental health. Dysbiosis has been linked to a host of mental and neurological disorders, including anxiety, depression, autism spectrum disorder, schizophrenia, and Alzheimer's disease.
Current Scientific Findings and Research
Current research is continually establishing the role of gut microbiota in managing mental health. Several studies have found that probiotics, known as 'good bacteria', can improve mental health by decreasing anxiety, depression, and stress levels. Moreover, increasing evidence suggests a strong relationship between certain dietary patterns, altered gut microbiota, and increased susceptibility to mental health disorders.
Maintaining Good Gut Health for Optimal Mental Health
Given the growing evidence supporting the intertwined nature of mental health and gut health, maintaining a healthy gut microbiome is a critical aspect of promoting mental health. Here are some recommendations on how to maintain a healthy gut microbiome:
- Eat a diversity of foods: A varied diet can lead to a diverse microbiome, which is good for your gut.
- Try fermented foods: Yogurt, kimchi, sauerkraut, and kefir are packed with beneficial probiotics.
- Consider a plant-based diet: Plant-based diets are high in fiber, which helps promote the growth of beneficial gut bacteria.
- Stay hydrated: Drinking plenty of water has been shown to benefit the mucosal lining of the intestines and promote the balance of good gut bacteria.
- Avoid unnecessary antibiotics: Overusing antibiotics can lead to antibiotic resistance and can harm your gut microbiome.
While we are still at the beginning of understanding the depth of the gut-brain axis, it is clear that gut health plays a crucial role in managing and maintaining mental well-being. This understanding opens up a range of possibilities for future health interventions targeted at improving gut health to promote positive mental health.






Comments
Leave a Comment